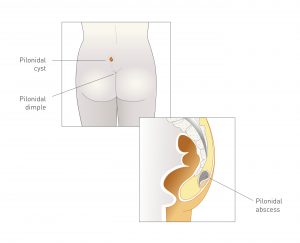
 Often described as a bump over the tailbone or between the buttocks, pilonidal disease results from hair impaction that can lead to a painful and localized infection. In its simplest form, pilonidal disease is asymptomatic, and may even remain so permanently. However, the condition requires close monitoring by an experienced colorectal surgeon who is trained to assess the need for further treatment.
Often described as a bump over the tailbone or between the buttocks, pilonidal disease results from hair impaction that can lead to a painful and localized infection. In its simplest form, pilonidal disease is asymptomatic, and may even remain so permanently. However, the condition requires close monitoring by an experienced colorectal surgeon who is trained to assess the need for further treatment.
When surgery is necessary to treat the pilonidal disease, the colorectal surgeons at La Peer Health Systems utilize an innovative procedure known as rhomboid flap excision. This clever surgical technique takes advantage of geometry and differing tissue tensions to achieve optimal closure and healing of operative site.
At La Peer Health Systems, our Los Angeles colorectal surgeons are trained in the most advanced surgical techniques to ensure the highest quality of care and optimal outcomes for our patients. To learn more about pilonidal disease or to find out if you are a candidate for this cutting-edge procedure, contact us today at (855) 360-9119 and ask to speak with our Department of Colorectal & General Surgery.
WHAT IS PILONIDAL DISEASE?
Pilonidal disease was first recognized during WWII, when military truck drivers began to suffer from pain, skin hardening, and discharge from cysts around the tailbone. It is now understood that a pilonidal cyst is caused by hair impaction into small openings in the skin, which lead to formation of a pilonidal cavity deep within the midline buttock tissue. Physical activities that place high shearing forces at the midline of the buttocks, such as sitting for long periods of time, can increase the risk of hair impaction. Other risk factors for pilonidal disease include:
- Excessive hairiness
- Increased sweating while sitting
- Poor personal hygiene
- Obesity
- Local trauma
TREATMENT OF PILONIDAL DISEASE
Treatment for a pilonidal cyst depends on the severity of discomfort and progression of the disease.
When a pilonidal cyst becomes infected it is first treated in the office with a simple incision and drainage. Under local anesthesia, an incision is made in the wound to allow for fluid drainage. This technique is used to treat the infection and provide symptomatic relief, but does not resolve the underlying disease.
Once the active infection is controlled, a formal excision can be performed. There are several techniques being used throughout the country. Most commonly, a surgeon removes all the disease tissue and leaves an open wound to heal over several months. This requires dressing changes a few times a day, and studies have demonstrated average wound healing rates between 6 – 21 weeks for full closure.
Given the extended period of time for healing with the leave open technique, flap closures have been employed to provide immediate recovery with no wound to care for over several months.
Excision with a rhomboid flap closure is performed under general anesthesia. A rhomboid-shaped excision is made of the infected site. Once the diseased tissue and infected debris has been removed, a skin flap of healthy disease free tissue is rotated and brought to close the entire defect.
Our specialty department, the Pilonidal Cyst Surgery Center of Excellence, offers a team of world-renowned surgeons who specialize in the most advanced treatment of pilonidal disease and pilonidal cysts.
ADVANTAGES OF THE RHOMBOID FLAP TECHNIQUE
Traditional approaches to pilonidal cyst excision involve either a simple primary closure or leaving an open wound. Simple closures can have failure rates as high as 50%, while open wounds take 2-3 months to heal at a minimum, while requiring daily wound management. Though a more technically challenging procedure, the rhomboid flap has distinct advantages for patients compared with the traditional surgical approach:
- Minimized wound infection rates between 7 – 10%
- Recurrence rate of approximately 4%, of the lowest reported in the literature
- Outpatient procedure (Return home the same day)
- Minimal wound-management for the patient
- Quicker return to normal daily activities
In the hands of the fellowship trained colorectal surgeons at La Peer, the rhomboid flap technique provides the greatest chance of both curing the disease and maximizing post-operative comfort.
FREQUENTLY ASKED QUESTIONS
Q: How common is pilonidal disease?
A: Pilonidal disease occurs in an estimated 0.7 percent of the population and is most common in post-pubertal young adults. The condition is rarely seen arising in individuals over the age of 40.
Q: When is surgery necessary?
A: When a pilonidal cyst becomes infected, incision and drainage of the affected area is the first step for treatment. This does NOT provide a cure. It will only control the infection. Once the infection has resolved, our colorectal surgeons recommend that a definitive surgical treatment be undertaken.
Q: What type of anesthesia is used during this procedure?
A: Surgical removal of a pilonidal cyst is typically performed under general anesthesia in our Beverly Hills outpatient center. You will not experience any pain or discomfort during the procedure and will be closely monitored by our staff during post-operative recovery.
Contact a Los Angeles Colorectal Surgeon
With timely diagnosis and proper care from an experienced colorectal surgeon, pilonidal disease is highly treatable. The team of surgeons at La Peer Health Systems come from some of the country’s most prestigious medical training institutions and are skilled in the most advanced procedures in the field of colorectal surgery.
If you believe you may have a pilonidal cyst, don’t hesitate to contact our Department of Colorectal & General Surgery today by calling (855) 360-9199 or filling out our online contact form. You can also learn more about treatment at our outpatient facility by visiting the Pilonidal Cyst Surgery Center of Excellence department website.
Next, read about Anal Fistulas.
